The New York Times
How to Spot Depression in Young Children
When parents bring their children in for medical care these days, there is no such thing as a casual, “Hey, how’s it going?” We doctors walk into every exam room prepared to hear a story of sadness and stress or, at the very least, of coping and keeping it together in this very hard year full of isolation, loss, tragedy and hardship, with routines disrupted and comfort hard to come by. Parents have carried heavy burdens of stress and responsibility, worrying about themselves but also watching their children struggle, and there is worldwide concern about depression and suicidality among young people. But it is not only the adults and the young adults and teenagers who are suffering and sad; young children can also experience depression, but it can look very different, which makes it challenging for parents — or doctors — to recognize it and provide help. Sign up for The Morning newsletter from the New York Times Rachel Busman, a clinical psychologist at the Child Mind Institute in New York City, said that it can be hard to think about depression in younger children because we picture childhood as a time of innocence and joy. But as many as 2% to 3% of children ages 6 to 12 can have serious depression, she said. And children with anxiety disorders, which are present in more than 7% of children ages 3 to 17, are also at risk for depression. Dr. Helen Egger, until recently the chair of child and adolescent psychiatry at NYU Langone Health, said that according to her public health research, between 1% and 2% of young children — as young as 3 — are depressed. Depression was originally conceived of as an adult problem. Maria Kovacs, professor of psychiatry at the University of Pittsburgh School of Medicine, said that in the 1950s and ’60s, there were child psychiatrists who believed that children did not have sufficient ego development to feel depression but that research she and other colleagues did in the ’70s showed that “school age children can suffer from diagnosable depression.” Before adolescence, depression is equally common in girls and boys, though among adolescents, it is twice as common in girls, and that predominance then lasts across most of adult life, until old age, when it again appears to equalize. What does depression look like in younger children? When young children are depressed, Kovacs said, it is not unusual for “the primary mood to be irritability, not sadness; it comes across as being very cranky.” And children are much less likely to understand that what they are feeling is depression or identify it that way. “It almost never happens that they say, ‘Something’s wrong because I’m sad,’” Kovacs said. It is up to adults to look for signs that something is not right, she said. The best way for parents to recognize depression in young children is not so much by what a child says as by what the child does — or stops doing. Look for “significant changes in functioning,” Kovacs said, like “if a child stops playing with favorite things, stops responding to what he used to respond to.” This might mean a child loses interest in the toys or games or jokes or rituals that used to be reliably fun or entertaining or does not seem interested in the usual back and forth of family life. “You’ve had a kid who was one way, and then you see that they’re more irritable and sad,” said Egger, who is now the chief medical and scientific officer at Little Otter, a new online mental health care company for children. Children may seem flattened, have less energy or tire easily. And they may start complaining about physical symptoms, especially stomachaches and headaches. They may sleep more — or less — or lose their appetites. A preschool-age child might be depressed if she is having daily tantrums, with behaviors that risk hurting herself or other people. Depression “may look like a behavior problem but is really being driven by what the kid is feeling inside,” Egger said. “It’s like walking through the world with dark-colored glasses,” Busman said. “It’s about myself, about the other person, and the world — I suck, this sucks, everything sucks.” Should I ask about suicidal thoughts? The irritability and the anger — or the flatness and the shutting down — can be signs of profound sadness. And while suicide attempts by elementary school-age children are rare, they do happen and have increased in recent years. Suicide was the second leading cause of death in children 10 to 14 in 2018, and a 2019 JAMA study showed increasing emergency room visits by children for suicidal thoughts or actions from 2007 to 2015 — 41% in children younger than 11. The presence of suicidal thoughts should be seen as a call for help. The most problematic myth about suicide is the fear “that if you ask about suicide, you’re putting the idea in their heads,” said Kovacs, who developed the Children’s Depression Inventory, which is used all over the world. “If you’re dealing with a child for whom this is not an issue, they’re just going to stare at you like you’re out of your head,” Kovacs said. “You cannot harm somebody by asking them.” But what if children say they have thought of suicide? As with adults, this suggests the child is living with pain and perhaps thinking about a way out. Kovacs said children may imagine death as “a release, a surcease, a relief.” Busman said that she works with children who may say, “I don’t want to kill myself, but I feel so bad, I don’t know what else to do and say.” If a child talks about wanting to die, ask what that child means and get help from a therapist if you are concerned. A statement like this can be a real signal that a child is in distress, so do not dismiss it or write it off as something the child is just saying for attention, she said. How can treatment help? “Parents should take child symptoms very seriously,” said Jonathan Comer, professor of psychology and psychiatry at Florida International University. “In serious forms, it snowballs with time, and earlier onset is associated with worse outcomes across the life span.” In a 2016 longitudinal study, Kovacs and her colleagues traced the course of depression starting in childhood and found recurrent episodes in later life. So if you see changes like withdrawal from activities, irritability or sadness, fatigue, or sleep disturbances that persist for two weeks, consider having the child evaluated by someone who is familiar with mental health issues in children of that age. Start with your pediatrician, who will know about resources available in your area. Parents should insist on a comprehensive mental health evaluation, Busman said, including gathering history from the parent, spending time with the child and talking to the school. An evaluation should include questions about symptoms of depression as well as looking for other problems, like attention deficit hyperactivity disorder or anxiety, which may be at the root of the child’s distress. Early treatment is effective, Comer said: “There’s terrific evidence for family-focused treatment for child depression; it focuses on family interactions and their impact on mood.” With children from 3 to 7, he said, versions of parent-child interaction therapy, known as PCIT, are often used — essentially coaching parents and helping them emphasize and praise what is positive about their children’s behavior. As much as possible, parents should try to keep children going outside, taking walks, even playing outdoor games, even if they are less enthusiastic about their usual activities. As with adults, physical exercise has both mental and biological benefits — as do fresh air and sunshine. Depression does not necessarily lend itself to simple cause-and-effect explanations, but Kovacs emphasized that with a first episode in a child, there is almost always a particular stressor that has set off the problem. It could be a change in the family constellation — a parental divorce, a death — or it could be something more subtle, like an anxiety that has spiraled out of control. If a child does begin therapy, part of the treatment will be to identify — and talk about — that stressor. How can I find help for my child? If you are concerned that your child might be depressed, start with your pediatrician or other primary care provider. Some clinics and health centers will have in-house mental health services, and you may be able to have your child seen there. Some doctors will have links to local therapists with experience with young children. Mental health specialists can be in short supply (and there is a lot of need right now), so be open to the possibility of care being delivered remotely, through telehealth. Kovacs also suggested that parents who are looking for treatment consider clinical psychology department clinics at a local university, where students in psychology and counseling are supervised by licensed psychologists; she said such clinics often have good availability. “Parents should see children’s struggles as opportunities to intervene,” Comer said. “The majority of early child mood problems will go away with time, sensitive parenting and supportive environments.” This article originally appeared in The New York Times. © 2021 The New York Times Company
Celebrities - Celebrities - Google News
April 12, 2021 at 05:36PM
https://ift.tt/2Rv26MT
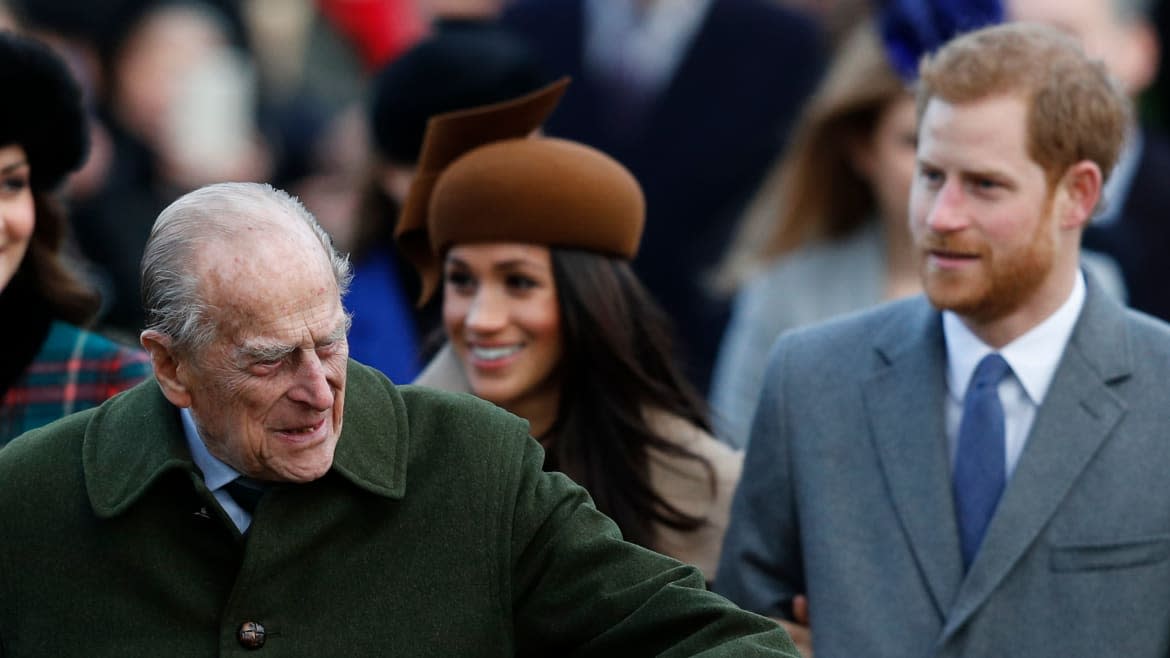
Prince Philip Thought Meghan Markle and Prince Harry’s Oprah Interview Was ‘Madness’ - Yahoo! Voices
Celebrities - Celebrities - Google News
https://ift.tt/2C2XYst
Bagikan Berita Ini















0 Response to "Prince Philip Thought Meghan Markle and Prince Harry’s Oprah Interview Was ‘Madness’ - Yahoo! Voices"
Post a Comment